Stage 3 Colon Cancer Survival Rate by Age
A diagnosis of stage 3 colon cancer can feel overwhelming, and one of the first questions that comes to mind is about survival rates.
The 5-year relative survival rate for stage 3 colon cancer is approximately 73%.
This means that people diagnosed with stage 3 colon cancer are, on average, about 73% as likely as people who don’t have that cancer to be alive five years after diagnosis.
However, this is a general statistic, and your personal outlook depends on many factors, with age being a significant one.
Receiving this diagnosis for yourself or a loved one brings a wave of questions and concerns. You’re likely searching for clear, reliable information to understand what this means for the future.
Statistics can feel cold and impersonal, but they are a crucial tool for doctors to understand the disease and plan the best possible treatment.
This guide is here to help you understand the survival rates for stage 3 colon cancer, specifically how they can vary by age.
We will break down the numbers, explain what they mean, and discuss other important factors that influence your prognosis.
Our goal is to provide you with the knowledge to have more informed conversations with your healthcare team.

What Does Stage 3 Colon Cancer Mean?
Stage 3 colon cancer means the cancer has grown through the wall of the colon and has spread to nearby lymph nodes.
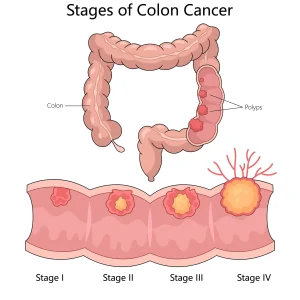
However, it has not yet spread to distant parts of the body like the liver or lungs. This is also known as regional-stage colon cancer.
Doctors further classify stage 3 into sub-stages (3A, 3B, and 3C) based on how far the tumour has spread and the number of lymph nodes involved.
- Stage 3A: Cancer has reached the inner or middle layers of the colon wall and spread to 1 to 3 nearby lymph nodes.
- Stage 3B: The cancer is more advanced, either by growing through the colon wall or involving more lymph nodes (up to 3).
- Stage 3C: Cancer has spread to 4 or more nearby lymph nodes, indicating a more advanced regional spread.
This classification is crucial because it helps doctors determine the intensity of treatment needed, which directly impacts the survival outlook.
How Does Age Affect Stage 3 Colon Cancer Survival Rates?

Yes, age is a significant factor in stage 3 colon cancer survival.
Generally, younger patients tend to have slightly better survival rates compared to older patients.
This is often because younger individuals may have fewer other health problems (comorbidities) and may be able to tolerate more aggressive treatments like chemotherapy.
However, it’s important to remember that these are just trends. A healthy and fit older person might have a better prognosis than a younger person with other serious health conditions.
⇒Survival Rates by Age Group
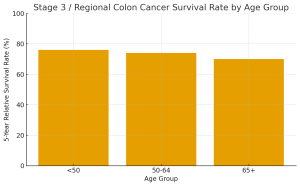
Here is a general breakdown of the 5-year relative survival rates for regional-stage colon cancer, which includes stage 3, by age group. These figures provide a clearer picture than a single overall statistic.
| Age at Diagnosis | 5-Year Relative Survival Rate (Regional Stage) |
| Younger than 50 | Approximately 76% |
| 50-64 | Approximately 74% |
| 65 and older | Approximately 70% |
These numbers show that while survival rates are slightly lower for older age groups, the outlook for patients over 65 remains quite positive. Advancements in treatment and supportive care have greatly improved outcomes for all ages.
What Other Factors Influence Survival Rates?
Besides age and the specific sub-stage, several other factors can influence a person’s prognosis with stage 3 colon cancer.
1. General Health and Fitness
Your overall health before diagnosis plays a major role. Patients who are fit and have no other serious medical conditions like heart disease or diabetes are often better candidates for surgery and chemotherapy. This can lead to better outcomes.
2. Treatment Response
How well your cancer responds to treatment is a critical factor. The standard treatment for stage 3 colon cancer is surgery to remove the tumour, followed by adjuvant chemotherapy to kill any remaining cancer cells.
A positive response to this combination therapy significantly improves the chances of a cure.
3. Tumour Characteristics (Grade and Biomarkers)
- Tumour Grade: This describes how abnormal the cancer cells look under a microscope. Low-grade tumours look more like normal cells and tend to grow slowly, while high-grade tumours look very abnormal and can be more aggressive.
- Biomarkers: Specific genetic markers in the tumour, such as MSI (microsatellite instability) or dMMR (deficient mismatch repair), can predict a better prognosis and may influence treatment choices.
4. Lifestyle Choices
Does making healthy lifestyle changes after diagnosis really matter? Yes, absolutely. Research suggests that maintaining a healthy weight, being physically active, and eating a balanced diet after treatment can lower the risk of cancer recurrence and improve overall survival.
Treatment Options for Stage 3 Colon Cancer
The primary goal of treatment for stage 3 colon cancer is to cure the disease. The standard approach involves a combination of surgery and chemotherapy.
- Surgery: The main treatment is a colectomy, where a surgeon removes the part of the colon containing the tumour along with nearby lymph nodes. This is a major operation, but it is essential for removing the primary cancer.
- Adjuvant Chemotherapy: After you recover from surgery, you will almost always be recommended chemotherapy. This is called ‘adjuvant’ therapy because it is given to destroy any microscopic cancer cells that may have escaped from the original tumour. This greatly reduces the risk of the cancer coming back. Common chemotherapy regimens include FOLFOX or CAPOX, usually given for 3 to 6 months.
For some rectal cancers (part of the large intestine), radiation therapy may also be used before or after surgery, often in combination with chemotherapy.
Stage 3 Colon Cancer Survival Story
A 52-year-old schoolteacher, Mr. Ramesh, received a diagnosis of stage 3 colon cancer, a moment that brought fear and uncertainty into his life.
Like many patients, his first concern was survival and whether treatment would give him a second chance.
Under the care of Dr. Aditya Kulkarni in Pune, his treatment plan included a successful surgery to remove the tumour and nearby lymph nodes, followed by a structured course of chemotherapy.
Despite the challenges, he completed every session with determination.
One year later, his follow-up scans remain clear, and he has returned to his classroom and daily routine with renewed confidence.
His journey is a reminder that even with a stage 3 diagnosis, timely treatment, the right medical guidance, and strong patient support can lead to an excellent recovery and hopeful future.
Key Takeaways
- The overall 5-year survival rate for stage 3 colon cancer is about 73%, but this varies.
- Age is an important factor, with younger patients generally having slightly higher survival rates. However, the prognosis for older adults is still very encouraging.
- Your specific sub-stage (3A, 3B, or 3C) is a crucial predictor of your outlook.
- Other factors like your general health, tumour characteristics, and response to treatment significantly impact survival.
- Standard treatment with surgery followed by chemotherapy offers a strong chance of a cure.
FAQs
1. Is Stage 3 colon cancer curable?
Yes. Stage 3 colon cancer is considered potentially curable in a large number of patients. With timely surgery and adjuvant chemotherapy, many people achieve long-term remission and never experience a recurrence. Cure rates are especially good when the tumour is completely removed and chemotherapy is completed as planned.
2. Can a 65–70-year-old with Stage 3 colon cancer still live 5 years or longer?
Yes. Many older adults do very well. Although survival percentages are slightly lower for those above 65, the actual outcomes depend more on overall fitness, heart and kidney function, and the ability to complete chemotherapy. A healthy 70-year-old can have outcomes similar to someone in their 50s if they respond well to treatment.
3. Why do survival rates slightly decrease with age?
Survival differences across age groups are mostly due to factors like slower healing, reduced immunity, and the presence of other medical conditions such as diabetes or heart disease. Older adults may also require chemo dose adjustments. However, age alone does not determine prognosis — overall health plays a much bigger role.
4. How long can someone live after Stage 3 colon cancer treatment?
Many people live 10, 15, or even 20+ years after treatment if the cancer does not recur in the first 5 years. Life expectancy is highly individual and depends on tumour biology, lymph node involvement, and treatment response rather than age alone. Long-term survival is very possible.
5. What is the risk of recurrence in Stage 3 colon cancer?
Recurrence risk varies based on sub-stage and lymph node involvement, but in general ranges between 20% and 40%. Stage 3A has the lowest recurrence risk, while Stage 3C carries the highest. Completing chemotherapy and attending regular follow-ups significantly lowers recurrence chances.
6. What symptoms should I watch for that may indicate recurrence?
Possible signs include changes in bowel habits, abdominal pain, unintended weight loss, persistent fatigue, or blood in stool. These symptoms do not always mean recurrence, but should be evaluated by a doctor to rule out any concerning changes.
7. How often should I go for follow-up after completing Stage 3 colon cancer treatment?
Follow-up schedules typically include doctor visits and blood tests every 3–6 months for the first 2 years, then every 6 months for the next 3 years. A CT scan is usually done once a year, and a colonoscopy is recommended 1 year after surgery, then every 3–5 years. Consistent follow-up helps in early detection of recurrence.
8. Does completing all cycles of chemotherapy improve survival?
Yes. Research shows that patients who complete their planned chemotherapy cycles have significantly better survival and lower recurrence rates. Even if dose adjustments are needed, maintaining continuity of treatment gives the best long-term results.
9. Do genetic or molecular tumour markers affect survival?
Yes. Tumours with MSI-high (MSI-H) or dMMR characteristics usually have a better prognosis. Mutations like KRAS or BRAF may influence recurrence risk and treatment choices. Molecular testing helps personalize treatment and gives a more accurate picture of survival.
10. Can lifestyle changes after treatment improve survival?
Absolutely. Maintaining a healthy weight, eating a balanced diet, exercising regularly, limiting alcohol, and avoiding tobacco all contribute to lower recurrence rates and better long-term survival. Small, consistent lifestyle habits make a meaningful impact.
11. What questions should I ask my doctor to better understand my personal survival outlook?
Useful questions include:
What was my exact sub-stage (3A, 3B, or 3C)?
How many lymph nodes were involved?
Do I need tumour genetic testing?
What is my individual recurrence risk?
How will chemotherapy improve my outcome?
Which lifestyle changes matter most for me?
These help you make informed decisions and understand your prognosis clearly.
12. Can Stage 3 colon cancer progress to Stage 4 later?
A Stage 3 cancer does not “turn into” Stage 4, but if cancer cells spread to distant organs later (such as liver or lungs), it is called metastatic recurrence, which is treated as Stage 4 disease. This is why regular follow-up and early detection are essential.
13.Are survival rates different for men and women in Stage 3 colon cancer?
There are slight differences, but they are not large. Some studies show that women may have marginally better outcomes due to hormonal and immunological factors, especially before menopause. However, survival primarily depends on sub-stage, age, lymph node involvement, tumour biology, and treatment — not gender alone.
14.Is the 73% survival rate accurate for everyone?
No. This number represents large groups, not individuals. Your personal prognosis can be much better or worse depending on:
-
Age
-
Sub-stage
-
Number of lymph nodes involved
-
Tumour grade
-
Biomarkers (MSI, KRAS, BRAF)
-
Response to chemotherapy
-
Lifestyle factors
Many Stage 3 patients live long, healthy lives far beyond 5 years.
15.How do survival rates differ between Stage 3A, 3B, and 3C colon cancer?

Dr. Aditya Kulkarni
MS, DNB, FRCS, MCh (Surgical Gastroenterology & GI Oncology)
Dr. Aditya Kulkarni is a Consultant of Laparoscopic and Robotic Gastrointestinal, Hepato-biliary-pancreatic, and Cancer Surgeon at the Renowned Oasis Surgery Clinic Pune.
